Key Takeaways
- Medicare does not cover abdominoplasty for cosmetic purposes, only for medically necessary reasons related to excess skin causing health issues.
- Eligibility for a Medicare-funded tummy tuck includes medical conditions like lower back pain, incontinence, muscle separation, hernias, and persistent skin infections.
- Candidates must demonstrate significant weight loss (at least 5 BMI points) and maintain stable weight for at least six months to qualify for coverage.
- Documentation from a surgeon is required to prove the medical necessity of the procedure to Medicare, including evidence of prior non-surgical treatments.
- Costs associated with the procedure may include surgeon, anaesthetist, and hospital fees, and patients should expect out-of-pocket expenses even with Medicare coverage.
Abdominoplasty and Medicare – Will Medicare Fund My Tummy Tuck?

- Want to know if Medicare will cover your surgery?
- Interested in the specific criteria for Medicare coverage?
- Want to know if your health fund with cover a Tummy Tuck?
This article covers the specific criteria for Medicare Cover of a Tummy Tuck or Abdominoplasty.
What is Abdominoplasty?
Abdominoplasty is a surgical procedure performed to remove excess skin and fat after pregnancy or weight loss. The abdominoplasty procedure can make your abdomen look more sculpted and well-defined. These new contours of your body are can help to improve your self-image and self-worth.
Abdominoplasty is more commonly known as tummy tuck and it can also be performed to remove excess skin after multiple pregnancies. A tummy tuck can improve the look of your body and give you the confidence to wear the type of clothing that you wish to. Research has also shown abdominoplasty can help relieve incontinence and posture problems.
You may be an ideal candidate for an abdominoplasty procedure if you have recently lost a significant amount of weight and are now maintaining a stable weight. Along with that, you should be a non-smoker and have realistic goals and expectations from the procedure. All of these criteria will be discussed during your consultation with Dr Mark Doyle, Specialist Plastic Surgeon.
Will Medicare cover my Abdominoplasty?
Medicare will only contribute to a portion of procedures performed due to medical reasons, hence, it does not cover abdominoplasty procedures for cosmetic purposes. Abdominoplasty or tummy tuck is a procedure that can improve the appearance of the body but also has medical benefits.
The presence of excess saggy skin can result in medical conditions like fungal infections in the skin folds or back problems due to the overhanging skin. These potential medical issues may make the tummy tuck procedure a medically necessary procedure. Now that it is a medical procedure, Medicare and your health insurance if you have any, will pay some money towards the costs of the abdominoplasty and other associated procedures if you meet the strict criteria. Please note that there will always be an out of pocket cost for these types of procedures. Costs associated with such a procedure will include surgeons fees, anaesthetist fees and hospital fees.
However, it is important for you to keep in mind that your surgeon will need to provide clear documentation to Medicare as evidence that this procedure is a medical necessity. Book a consultation with Dr Mark, specialist plastic surgeon to find out if you qualify for a medically necessary tummy tuck or panniculectomy procedure.
Eligibility Criteria for Medicare Funded Tummy Tuck Procedure
You may be eligible for a partly medicare-funded tummy tuck procedure if you suffer from any of the following medical issues;
- Lower Back Pain: Researchers have shown that the excess skin and weakness of muscles of the abdominal wall can exert pressure on the lower back, resulting in excruciating and constant lower back pain. This pain has been shown to improve significantly after the abdominoplasty procedure.
- Incontinence: Mums who have given birth to twins or have has more than two children with different pregnancies often suffer from excess skin and incontinence that can reduce their quality of life. These health impairments however can be fixed with the tummy procedure and medicare is more than likely to fund the procedure. It is important to keep in mind that Medicare does not cover any abdominoplasty performed that is only due to excess skin as a result of pregnancy. It is likely that Medicare will cover part of your tummy tuck procedure after pregnancy if there are actual medical reasons for it, but you need to speak to your plastic surgeon to find out more.
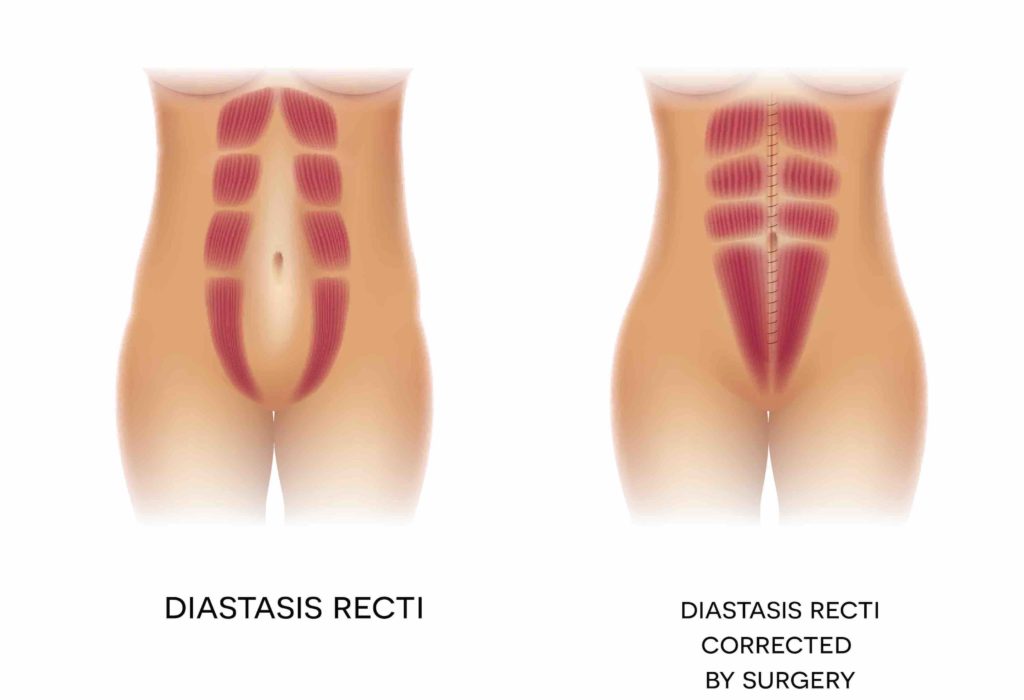
- Muscle Separation (Diastasis Recti): Muscle injury, separation, and laxity are common in mums and people who have lost massive amounts of weight. This muscle injury and weakness can result in actual medical issues, hence, an early repair is necessary. They can be easily repaired using a tummy tuck procedure which is, at least partly, going to be covered by medicare.
- Hernias: Muscle weakness has the potential to cause a hernia when combined with other predisposing factors. A tummy tuck procedure can reduce the hernia and reduce the risk of any other hernia developing. Talk to Dr Mark to know more about hernias, muscle weakness, and Medicare-funded abdominoplasty procedure.
- Skin Rashes and Infections: Having excess skin with multiple skin folds allows fungi and other microorganisms to grow in them, resulting in severe skin infections and rashes. If persistent, these can cause medical complications and hence, should be treated immediately. If you undergo the removal of excess skin due to persistent or recurring skin infections, rashes, and irritation of the skin folds, the procedure may be covered by Medicare.
However, you should keep in mind that you have to have tried non-surgical methods of treating the skin infections and rashes, for at least three months with no result for you to be eligible for a Medicare-funded tummy tuck procedure.
For Medicare to cover your tummy tuck procedure, you must have lost a significant amount of weight, which is defined as losing at least 5 BMI points. Basically, if you have lost around 10 kgs to 15 kgs of weight in a short period of time, you may be eligible for a medicare funded tummy tuck procedure.
Another important eligibility criteria is that you must maintain a steady weight after losing weight to be considered for Medicare coverage. You must maintain a steady weight with minimal fluctuations for at least six months. If you can’t show that you have achieved a stable weight, then the chances of getting your procedure covered by Medicare are reduced.
You will also need to prove that the excess skin is affecting your daily life and non-surgical treatments have not yielded any positive results.
What Medicare Item Numbers Cover a Tummy Tuck Procedure?
- 30177: Lipectomy, Post Weight loss Tummy Tuck (Abdominoplasty)
- 30179: Circumferential lipectomy (Belt lipectomy) – used for massive weight loss excess skin removal
- 30172: Lipectomy – multiple wedges of skin removal after Weight loss (for a Tummy Tuck)
- 30165: Lipectomy, wedge excision of abdominal apron that is a direct consequence of significant weight loss. This applies to people with excess skin that hangs over their abdomen and pubic region like an apron.
- 30168: Lipectomy, wedge excision of redundant non-abdominal skin and fat that is a direct consequence of significant weight loss. This applies to the procedure where only 1 excision is made and includes areas of the body like arms, legs, and so on. (e.g. Arm lift and Leg lift)
It is important to note that these numbers are subject to change and you should speak to your doctor in-depth and research the MBS online criteria to make sure that the numbers have not changed.
Basic Criteria and Requirements for these Medicare Item Numbers
- 30177: Lipectomy, excision of skin and subcutaneous tissue associated with redundant abdominal skin and fat that is a direct consequence of significant weight loss, in conjunction with a radical abdominoplasty (Pitanguy type or similar), with or without repair of musculoaponeurotic layer and transposition of the umbilicus, not being a service associated with a service to which item 30165, 30168, 30171, 30172, 30176, 30179, 45530, 45564 or 45565 applies, if: (a) there is intertrigo or another skin condition that risks the loss of skin integrity and has failed 3 months of conventional (or non-surgical) treatment; and (b) the redundant skin and fat interferes with the activities of daily living; and (c) the weight has been stable for at least 6 months following significant weight loss prior to the lipectomy.
- 330179: Circumferential lipectomy, as an independent procedure, to correct circumferential excess of redundant skin and fat that is a direct consequence of significant weight loss, with or without a radical abdominoplasty (Pitanguy type or similar), not being a service associated with a service to which item 30165, 30168, 30171, 30172, 30176, 30177, 45530, 45564 or 45565 applies, if: (a) the circumferential excess of redundant skin and fat is complicated by intertrigo or another skin condition that risks loss of skin integrity and has failed 3 months of conventional (or non-surgical) treatment; and (b) the circumferential excess of redundant skin and fat interferes with the activities of daily living; and (c) the weight has been stable for at least 6 months following significant weight loss prior to the lipectomy (H)
- 330172: Lipectomy, wedge excision of redundant non-abdominal skin and fat that is a direct consequence of significant weight loss, not being a service associated with a service to which item 30165, 30168, 30171, 30176, 30177, 30179, 45530, 45564 or 45565 applies, if:(a) there is intertrigo or another skin condition that risks loss of skin integrity and has failed 3 months of conventional (or non-surgical) treatment; and (b) the redundant skin and fat interferes with the activities of daily living; and (c) the weight has been stable for at least 6 months following significant weight loss prior to the lipectomy; and (d) the procedure involves 3 or more excisions (H) (Anaes.) (Assist.)
What to Expect while getting Medicare Coverage
You should be prepared to fill in the paperwork and spend time on the phone to get the medicare rebates for your procedure. You will need to meet the eligibility criteria, with actual evidence.
The evidence here is documentation from your doctor that you have tried other non-surgical methods to improve the quality of life with little to no results. You will also need to provide proof that you haven’t had weight fluctuations in the last six months.
You should also know that Medicare or any other insurance provider will not completely fund your procedure. This means that there may be some additional costs that you will have to pay out of your pocket.
Will my Private Health Insurance Cover an Abdominoplasty / Full Tummy Tuck?
If you get Medicare coverage then you may be eligible for Private Health Insurance coverage too. It is very important for you to check your health insurance coverage plan as each plan is unique and different from other funds. You will typically need GOLD level cover to be funded for most plastic surgery. Hospital costs can be very expensive with this procedure but are often covered by health insurance if there is medicare coverage.
Associated Medical Procedures Funded by Medicare
Medicare generally covers any procedure that is medically necessary and results in improved health. This may include certain other plastic surgery procedures, but they usually have very strict eligibility criteria that you will need to meet. Moreover, it is usual that the entire procedure won’t be covered but rather just part of it.
Some of the many plastic and reconstructive procedures that have Medicare rebates are mentioned below:
- Breast Reduction and Breast Lift (if you meet the criteria)
- Labiaplasty (if you meet the criteria)
- Excess Skin Removal after massive weight loss (if you meet the criteria)
- Breast reconstruction after a mastectomy due to breast cancer
- Skin Reconstruction and plastic surgery in burn patients
- Excess Eye Skin removal (Blepharoplasty surgery) to improve vision, which may also improve facial aesthetics the appearance of the eye
- Cleft Lip and Palate Surgery
- Treatment of birth defects and malformations that impair the proper functioning of the body.
Frequently Asked Questions

Are mums eligible for a Medicare-covered Tummy Tuck Procedure?
Unfortunately, the post-pregnancy tummy tuck procedure for saggy stretched tummy skin is rarely covered by Medicare as it is not seen as medically necessary and has few medical consequences. However, if you are thinking of undergoing a surgical procedure due to separation of muscles or urinary incontinence due to pregnancy, then there is a chance that Medicare may cover part of your procedure. Talk to you Dr Mark to find out more.
Will I need to be hospitalised after the procedure?
Abdominoplasty procedure can be an outpatient procedure, but most patients are kept in the hospital overnight for monitoring and you will be discharged the next day. Your private health insurance may help cover your hospital costs if you meet the Medicare coverage criteria.
You need to discuss this with your surgeon and health insurance company before undergoing the procedure.
How long will the Tummy Tuck procedure take?
An Abdominoplasty procedure takes anywhere between two hours and three hours depending on the amount of excess skin and consequently, the type of abdominoplasty procedure you are undergoing.
Are there any associated procedures to the Abdominoplasty procedure?
The Abdominoplasty procedure is performed for the purpose of removing excess skin from your abdominal region and to help make it look firmer and sculpted. Commonly, liposuction, which is a body sculpting procedure that helps remove some stubborn fat, is often performed at the same time to improve abdominal contours.
Book a Consultation
If you’d like to find out more, book a detailed consultation with Specialist Plastic Surgeon, Dr Mark Doyle.
Further Reading
- Visit the MBS Online – Medicare Item Number details
Related Blogs
About Dr Mark Doyle FRACS (Plas) – Queensland Plastic Surgeon
Servicing patients in Gold Coast, Brisbane, Sunshine Coast, Cairns and New South Wales NSW – Northern Rivers, Byron Bay, Ballina, Lismore and more.
Dr Mark Doyle is a fully qualified Specialist Plastic Surgeon with over 30 years of experience performing breast, body, face and nose surgery. He has completed all required training and only carries out approved surgical practices. There are NO undertrained doctors or cosmetic doctors acting as surgeons at Gold Coast Plastic Surgery.

